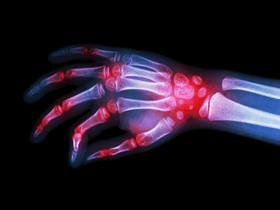
Rheumatoid arthritis is a condition that causes chronic inflammation. Like other types of arthritis, it affects the joints.
However, it can also affect the organs and tissues, such as the skin, blood vessels, heart, lungs, and eyes. Rheumatoid arthritis is an immune system disorder.
It occurs when the immune system incorrectly identifies the body’s own tissues as a threat and attacks them.
Unlike osteoarthritis, rheumatoid arthritis is not caused by everyday wear and tear on the joints.
The disease typically affects the lining of the joints. Over time, swelling and inflammation can erode the bones and cause deformation.
In some cases, the inflammation caused by rheumatoid arthritis damages other parts of the body as well.
Though medication and treatment options are available, rheumatoid arthritis can cause physical disabilities in severe cases.
Seropositive and Seronegative Rheumatoid Arthritis
Not so long ago, different types of rheumatoid arthritis were not recognized. When rheumatoid arthritis was diagnosed, it was always treated in the same way.
As research progressed, some experts began to see rheumatoid arthritis as a group of diseases.
Within this group, genetic differences between individuals affect the features, symptoms, and triggers of the disease.
These differences may be able to help doctors improve treatments for rheumatoid arthritis, and in some cases, even prevent the disease altogether.
The difference that researchers currently know the most about is between seropositive and seronegative rheumatoid arthritis.
Seropositive Rheumatoid Arthritis
When testing for seropositive rheumatoid arthritis, a blood test shows the presence of rheumatoid factor (RF) or anti-cyclic citrullinated protein antibodies (ACPAs). These antibodies are produced in the body and are present in between 60 and 80 percent of people diagnosed with RA.
Research has shown that these antibodies are often present between 5 and 10 years prior to the appearance of symptoms.
For people who have symptoms of rheumatoid arthritis and who also test positive for RF or ACPA, a diagnosis of rheumatoid arthritis is highly likely.
Seronegative Rheumatoid Arthritis
Some people with symptoms of rheumatoid arthritis do not test positive for RF or ACPA. This is known as seronegative rheumatoid arthritis.
Research suggests that approximately 38 percent of people with rheumatoid arthritis are seronegative.
Seronegative rheumatoid arthritis is more difficult to diagnose since there is no test for it. Instead, doctors must rely on symptoms to diagnose the disease. Your doctor might look for key symptoms, including:
- Stiffness that usually appears in the morning and affects the feet, ankles, knees, hips, elbows, or knees. Stiffness should typically last for more than an hour and appear for at least six consecutive weeks.
- Swelling, tenderness, pain, or redness in the joints. Rheumatoid arthritis typically affects joints symmetrically on both sides.
- Symmetrical symptoms in more than one joint.
- Ongoing inflammation
- Fatigue
Key Differences:

Aside from the presence or absence of RF and ACPA, researchers have identified other differences in the features and symptoms of these two types of rheumatoid arthritis.
Researchers once believed that patients with seropositive rheumatoid arthritis had more intense symptoms. However, recent studies suggest that this might not be the case. Instead, there might be a difference in which joints are affected.
More studies are needed to understand these differences and how they affect long-term outcomes.
Can Seronegative Rheumatoid Arthritis Become Seropositive?
People who test negative for RF and ACPA may become positive later on. Up to 80 percent of people with seronegative rheumatoid arthritis will eventually become seropositive.
Doctors say that this change typically happens within two years of receiving a diagnosis.
Some cases initially diagnosed as seronegative rheumatoid arthritis will later be diagnosed with other autoimmune disorders, such as psoriatic arthritis or chronic gout.
Seronegative rheumatoid arthritis is more likely to be incorrectly diagnosed than seropositive arthritis. Its symptoms can bear a resemblance to those associated with osteoarthritis.
In other cases in which seronegative rheumatoid arthritis is diagnosed, it may not respond to conventional treatments.
That may be a sign that the patient doesn’t actually have seronegative rheumatoid arthritis, but another condition altogether.
Other types of arthritis, including spondyloarthritis, which affects the spine, can be mistaken for rheumatoid arthritis.
Risk Factors
Seropositive and seronegative rheumatoid arthritis have similar risk factors. For instance, women are more likely to develop rheumatoid arthritis than men.
In addition, the disease is more common among people who are between 40 and 60 years of age with a family history of rheumatoid arthritis.
Smoking cigarettes, obesity, and exposure to certain environmental chemicals are other prominent risk factors.
Treatments

Treatments for both seronegative and seropositive rheumatoid arthritis are similar. In both cases, the objective of treatment is to help the patient manage pain and slow or prevent the progression of the disease.
Common treatments include:
- Medications to treat pain and inflammation and slow the progression of the disease
- Physical or occupational therapy to maintain joint health
- Surgery to repair damaged joints, reduce pain, and correct joint deformities
- Alternative medicine to complement treatment and improve overall health
The information in this article should not be taken as professional medical advice. If you are having issues or have health-related concerns, you should see your personal physician
This page is also available in:
![]() English
English